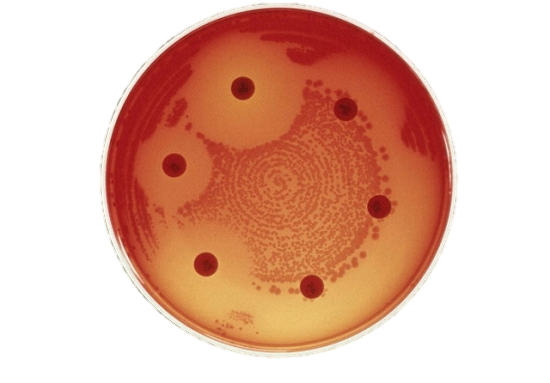
AMR Petri dish
With antimicrobial resistance (AMR) threatening development and health in Africa, six international and continental organizations are launching the first partnership of its kind to combat this public health crisis on the continent.
The partners cemented their collaboration today with a joint statement by eight senior representatives on the first day of the World Antimicrobial Awareness Week (WAAW) Campaign for Africa, noting the “silent public health threat that AMR poses in all countries in Africa” and expressed concern for the “uncontrolled antimicrobial use across the African continent.”
Antimicrobials include antibiotics, antivirals, antifungals and antiprotozoals and are used to prevent and treat infections in humans, animals, and plants. Antimicrobial agents have saved millions of lives, protected animal health and welfare as well as food security. But their rampant misuse in health settings and agriculture is killing 700 000 people annually around the world. In Africa, research findings estimate that 4.1 million people could die of failing drug treatments by 2050 unless urgent action is taken.
While data on AMR are sorely lacking on the continent, there are signs that resistance to commonly prescribed antimicrobials is significant. Malaria, which kills 3000 children in Africa every day, is increasingly showing resistance to once-effective treatment options. Tuberculosis is becoming resistant to the drugs typically used to treat it. Current studies indicate that drug resistance to HIV is increasing and could cause 890 000 deaths by 2030 in Sub-Saharan Africa.
AMR is exacerbated by the easy availability of medicines without a prescription. An estimated one in ten medicines globally is substandard or falsified, and the African Region is affected more than other parts of the world. In markets and on street corners, people are buying antimicrobials of unknown quality. Without proper medical supervision, people often stop their drug course too soon or they double-dose rather than keep to a prescribed strict time interval for appropriate drug-taking. The same happens in treatment of animal diseases coupled with underdosing, disrespect to drug withdrawal periods, and use of antimicrobials as growth promoters.
The improper use of antimicrobial medicines enables bacteria, viruses, fungi and protozoa to mutate into superbugs that are resistant to the drugs designed to kill them. These superbugs can travel across countries, resulting in thousands, or potentially millions, of deaths. Their treatment is resulting in prolonged hospital stays and the need for more expensive medicines, leading to huge additional costs in health expenditure by governments and individuals. The World Bank projects that the additional health care cost by 2050 could be between US$ 0.33 trillion and US$ 1.2 trillion.
AMR in Agriculture reduces productivity, hinders the provision of safe food and has a direct impact on food security and sustainability of livelihoods for farming communities. Improper disposal of pharmaceutical, hospital, abattoir, human and animal wastes contaminates the environment with antimicrobials and antimicrobial resistant organisms.
AMR is not only a health issue but a complex problem that requires a united multisectoral approach. The six partners making this joint statement represent the public health, agriculture, animal health and environmental sectors.
The organizations jointly committed to 10 points of actions, including fostering a One Health approach and leveraging each organization’s core competencies. The other areas of collaboration include
Accra, Addis Ababa, Bamako, Brazzaville, Cairo, Nairobi, 18 November 2020